- Olecranon fractures are common injuries affecting the elbow joint due to olecranon located subcutaneously where it is vulnerable to injury
- These fractures are diagnosed clinically and by elbow X rays
- Treatment is operative in most cases
Mechanism of injury
- Olecranon fractures are caused by Multiple mechanisms, those include:
- Low energy trauma (e.g. a fall on the outstretched hand, fall on the elbow)
- High energy trauma to the elbow (e.g. road traffic accidents)
- Stress fracture due to long periods of stress on the bone in athletes
Anatomy of proximal ulna
- Ulna is medial and longer forearm bone
- Ulna has a big proximal end (compared to the radius which has a smaller one), ulna proximal end articulate with the humerus proximally and the head of the radius laterally
- Ulna articulates with the humerus with two processes (projections), which include the coronoid process and the olecranon process
- The anterior process is the coronoid process which projects anteriorly and insert into the coronoid fossa during full elbow flexion
- The posterior process is the olecranon, which serves as a short lever for extension of the elbow
- The olecranon and coronoid processes form the walls of the trochlear notch which articulate with the trochlea of the humerus
- On the lateral side of the coronoid process is a smooth rounded concavity which is called the radial notch and it is where the radial head articulates with the ulna
- The triceps tendon inserts into the olecranon
- Inferior to the coronoid process is the tuberosity of the ulna which is the insertion of the brachialis tendon
- The shaft of the ulna is thick proximally but its diameter diminishes as it continue distally
Classification
- Mayo classification is the most commonly used classification for olecranon fractures, and it classify these fractures according to displacement, comminution and elbow joint stability
- Mayo classification on three types:
- Type 1
- Type 2
- Type 3
- Type 1: undisplaced
- A: Non comminuted
- B: Comminuted
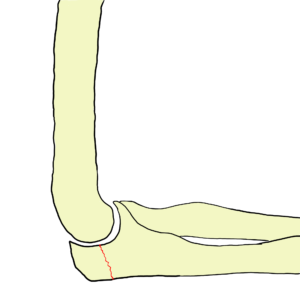

- Type 2: Displaced > 3mm olecranon fractures with a stable elbow joint
- A: Non comminuted
- B: Comminuted


- Type 3: Displaced > 3mm olecranon fractures with dislocated elbow joint
- A: Non comminuted
- B: Comminuted


Clinical features
- Symptoms
- Patient present with elbow pain and patient can localize the pain to posterior elbow
- Think of olecranon stress fracture if the patient gives a history of a pain during a long period of time
- Physical examination
- Look
- Elbow swelling
- Ecchymosis on posterior elbow
- Deformity if there is associated elbow dislocation
- Feel
- there is tenderness on pressure over posterior elbow
- Displaced fragment can be felt
- Move
- Patient can’t extend elbow against gravity
- Look
Imaging
- X-rays
- AP and lateral elbow X rays are ordered
- Note the fracture pattern, fracture comminution, presence of displacement and elbow joint condition (dislocated or not)
- CT helpful in preoperative planning

Emergency management
- Pain management
- In Injuries associated with elbow dislocation (Mayo III), the elbow should be reduced
- An above elbow backslab and collar and cuff is provided to Mayo I and II injuries and Mayo III after reduction
Definitive Management
- Non operative
- Operative
Non operative
- Indications:
- Mayo 1: elbow X rays should be taken when the elbow in flexion to make sure no displacement
- Mayo 2 in elderly patients > 70 years old only. as a result, patient lose some of the elbow extension power but that is much better than experiencing the operative complications at this age
- Non operative treatment consist of cast immobilization at 45-90 and exercises are started at 1 week
Operative
- Indications
- Mayo 2 in patients younger than 70 years old
- All Mayo 3 fractures
- Mayo 2 A treated with tension band wiring, Mayo 2 B and Mayo 3 treated with olecranon plating
- Immediate post operative mobilization is recommended to prevent stiffness
Complications
- Fixation hardware irritation to the subcutaneous border of olecranon (common)
- Elbow stiffness: occur in 50% of patients and minimized by early mobilization
- Non union: due to inadequate reduction and fixation. Treated with ORIF if elbow function is bad
- Ulnar nerve symptoms: resolve spontaneously in most cases
- Osteoarthritis: late complication, occur in 20% of patients and treated with analgesia
- Wound infection
Course Menu
This article is apart from The Elbow and Forearm Trauma Free Course; This course contains a number of lectures listed below:




