- Distal humerus fractures account for about 2 % of all fractures in adults
- They have a bimodal distribution in young males due to high energy injuries, and elderly females with osteoporosis due to low energy trauma
- These fractures can be very difficult to manage because they might involve the articular bone
Anatomy of distal humerus
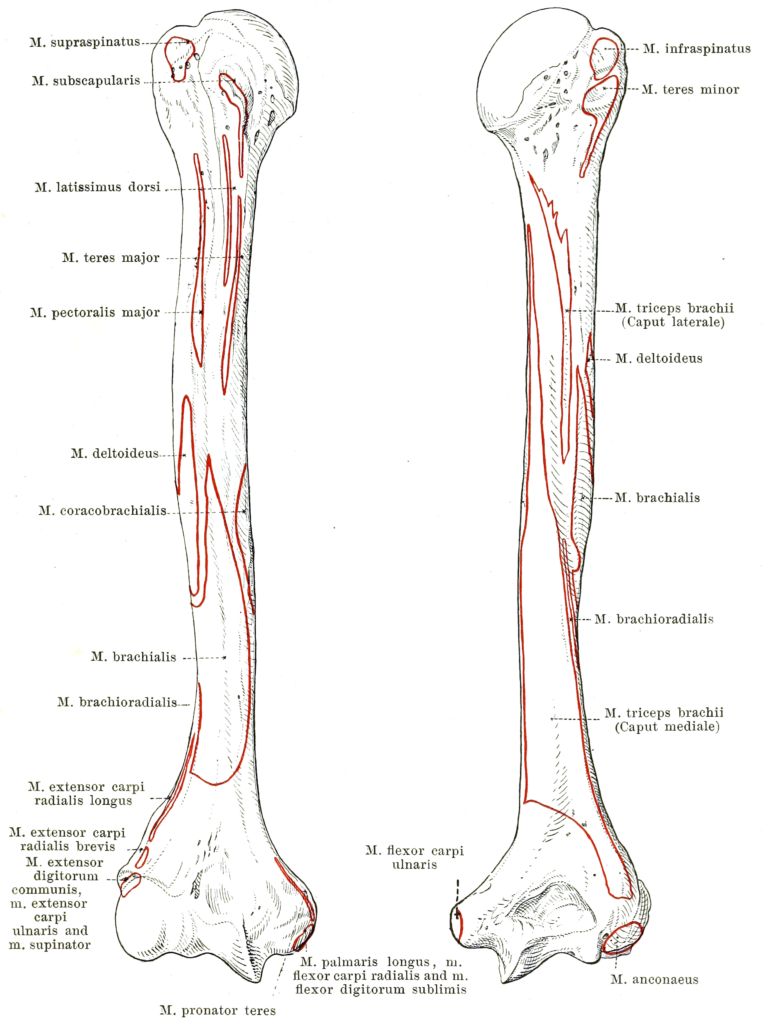
- The inferior end of the humeral shaft gradually widens to form the medial and lateral supracondylar ridges which then terminate in the medial and lateral epicondyles providing muscle attachment
- The condyle has two articular surfaces: a lateral capitulum which articulate with the radial head and a medial trochlea which articulate with the ulna

- Superior to the articular surfaces, there is three fossae (three bony depressions)
- Two of them are anterior, and those are the coronoid fossa and the radial fossa
- Coronoid fossa receives coronoid process of ulna during full flexion and radial fossa receives the edge of the radial head during full flexion of the elbow
- The third fossa is located posteriorly, and it is the olecranon fossa which receives the olecranon process of the ulna during full extension of the elbow
- Distal humerus articulate with proximal radius and ulna to form the elbow joint
Neurovascular structures
- Brachial artery provides blood supply to the arm and it is a continuation to the axillary artery
- Brachial artery lies anterior to the brachialis muscle and it accompanies the median nerve in its course
- Brachial artery is at risk of getting injured during distal humerus fractures
- Three main nerves are crossing the elbow and at risk of getting injured during distal humerus fractures, those include:
- Median nerve travels medial to brachial artery and passes between the two heads of pronator teres and it continuous to supply most of the flexors in the forearm (anterior)
- Ulnar nerve travels behind the medial epicondyle of the humerus (can easily get injured)
- Radial nerve crosses anterior to lateral epicondyle between brachialis and brachioradialis muscles and continuous to supply the extensors compartments in the forearm (posterior)
- Tests are done to make sure these nerves are not injured
Mechanism of injury
- Low energy trauma: from falls on the arm with the elbow flexed, or direct blow to the elbow or from indirect valgus or varus trauma to the arm while the elbow extended
- High energy trauma: motor vehicle accidents and crush injuries
Classification
- The AO classifies distal humeral fractures according to articular involvement, number of fragments, affected segment (trochlea, capitellum, epicondyles), plane of the fracture (sagittal, coronal) and height of the transverse fracture (transcondylar, supracondylar) into three types:
- Type A: extra-articular
- Type B: partially intra-articular
- Type C: completely intra-articular
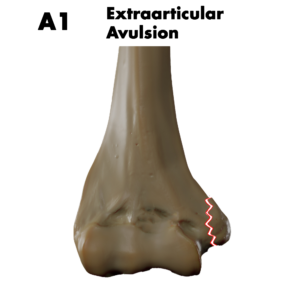
Type A
- Type A: extra-articular distal humerus fracture and it is subclassified into:
- A1: medial or lateral epicondyle avulsion fracture
- Type A:
- A2: simple extra articular distal humerus fracture, simple fractures examples include spiral, oblique or transverse
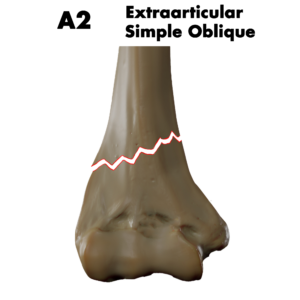
- Type A:
- A3: intact wedge, fragmentary wedge or Multi fragmentary extra-articular distal humerus fracture
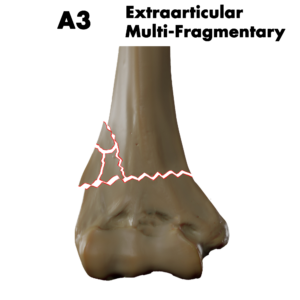
Type B
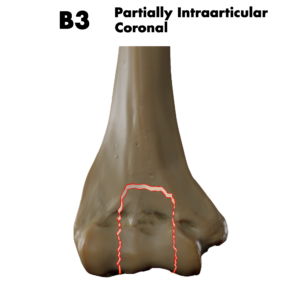
- Type B: partially intra-articular distal humerus fractures and it is subclassified into:
- B1: lateral sagittal fracture: e.g. simple transtrochlear fracture, capitellum fracture, fragmentary transtrochlear fracture
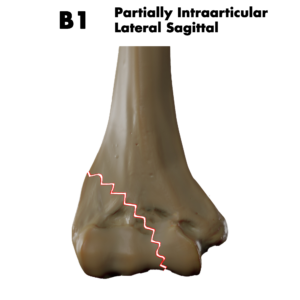
- Type B:
- B2: medial sagittal fracture: e.g. simple transtrochlear fracture through the medial articular surface , simple trantrochlear fracture through the trochlear groove, fragmentary transtrochlear fracture
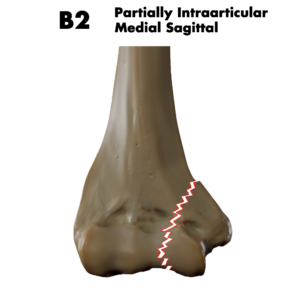
- Type B:
- B3: coronal plane fracture, e.g.: capitellum fracture, trochlea fracture, capitellum and trochlea fracture
Type C
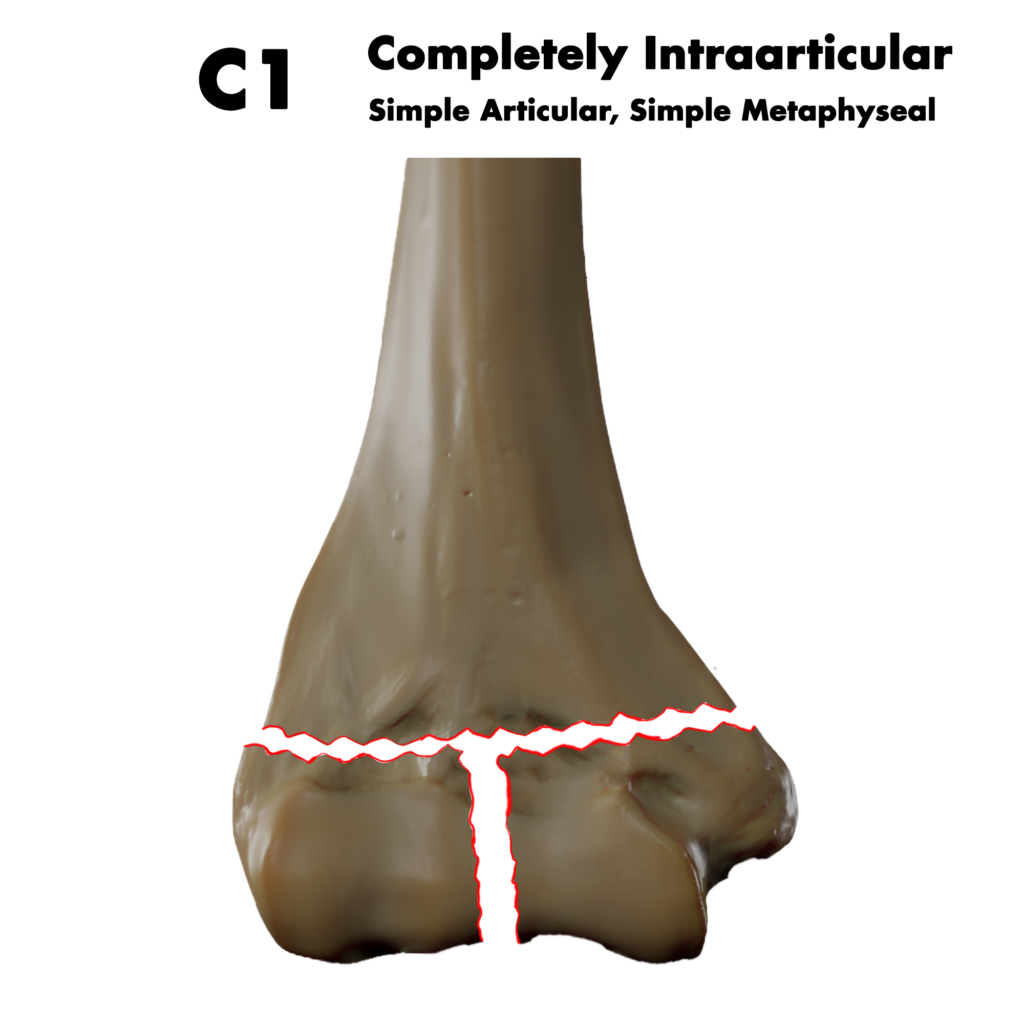
- Type C: completely intra-articular distal humerus fractures:
- C1: simple articular, simple metaphyseal fracture
- The metaphyseal fracture is furtherly classified into at the level of condyles, or above the level of condyles
- Type C:
- C2: simple articular, wedge or multifragmentary metaphyseal fracture, subclassified into: intact wedge fracture, fragmentary wedge fracture, multifragmentary fracture
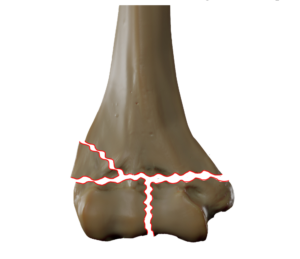
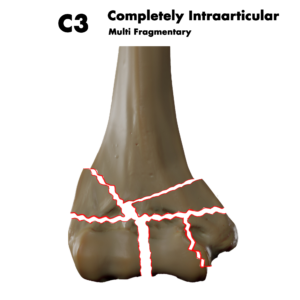
- Type C: completely intra-articular distal humerus fractures:
- C3: multifragmentary articular fracture, wedge or multifragmentary metaphyseal fracture, subclassified into: simple metaphyseal fracture, wedge metaphyseal fracture, multifragmentary metaphyseal fracture
Clinical features
- Patient present complaining of pain and swelling of the elbow after some type of trauma
- deformity might be present
- Bruising around the injured area might not be present initially but will develop few hours after
- Patient can’t move their elbow
- Injury to the brachial artery will result in expanding hematoma rather than dysvascular limb due to the rich collateral circulation around the elbow
- Careful neurological examination for the three main nerves (median, ulna and radial) to exclude injury
Imaging
- AP and lateral elbow radiographs are ordered and they are enough to make the diagnosis
- they shows most of the distal humerus fractures well except it is hard to tell whether on or both condyles are involved, especially when one or both of them are not displaced and it is hard to detect the comminution of intercondylar bone
- CT scans can be helpful in planning the surgical treatment in complex fractures

Emergency management
- Pain management
- Deformed limb should be reduced, and above elbow backslab is used to stabilize the limb, limit pain until definitive management is decided
- Reassessment for neurovascular injuries is done after applying the slab to make sure there is no injuries
Definitive management
- Non operative
- Operative
Non operative management
- Minimally displaced fractures are treated non operatively in some cases
- Non operative treatment consist of a applying a cast or a splint for 6 weeks with repeating the imaging after 1 week of treatment to make sure no displacement occur
- Displaced fractures in patient with poor bone quality (elderly) are also managed non operatively (can’t be fixated) or in patients who are unfit for surgery, the aim is to create a painless pseudarthrosis and mobilize early => prognosis is bad
- The danger with conservative treatment is strong tendency to stiffening of the elbow and persistent pain
Operative management
- Most distal humeral fractures are managed operatively since immobilization of one week or longer (in non operative therapy) lead to stiffness and poor functional outcomes
- The goal of operative treatment is anatomical reconstruction of the articular surface and stabilize it well to allow for early mobilization and prevention of stiffness
- So Displaced and minimally displaced distal humerus fractures are managed operatively in most cases, options include:
- ORIF: most of displaced fractures are fixated with plates
- Fragment excision: small fragments excised because it is too small to be fixated and to avoid restriction of movement done by that fragment
- Elbow arthroplasty: low transcondylar fracture in patient with osteoporosis maybe best treated with arthroplasty
- Distal humerus is approached from the posterior aspect utilizing one of the following techniques:
- Triceps splitting
- Triceps sparing
- Olecranon osteotomy
Notes
- Prolonged immobilization will result in elbow stiffness
- Early movement is the primary objective of treatment
Other indications of surgery
- Surgery is also indicated in:
- Neurovascular compromise
- Open fractures => if there is soft tissue contamination then treated with external fixation
Complications
- Vascular injury
- Early complication
- Excluded by testing the radial and ulnar pulses and capillary refill time distal to the injury
- Injury to the brachial artery will result in expanding hematoma rather than dysvascular limb due to the rich collateral circulation around the elbow
- Nerve injury
- Ulnar nerve is the most common nerve (50%) to get injured in these fractures and it also can be injured during operative treatment, radial nerve to a lesser degree and median nerve is rarely injured
- It is important to examine the hand and record findings before and after treatment
- Loss of reduction: repeating the X rays is important to make sure reduction is not lost
- Infection: hard to treat
- Elbow stiffness
- Late complication
- Stiffness is a common complication after distal humerus fractures
- Cause of elbow stiffness maybe intrinsic (intra articular adhesions, capsular contracture, joint incongruity, instability) or extrinsic (heterotopic ossification or nerve entrapment)
- Patient complain of loss of motion, particularly terminal extension
- Prevention of elbow stiffness is by early mobilization of the joint after the injury
- Elbow arthrolysis is one of the treatment options for elbow stiffness
- Non union
Course Menu
This article is apart from The Elbow and Forearm Trauma Free Course; This course contains a number of lectures listed below: